What is Colorectal Cancer?
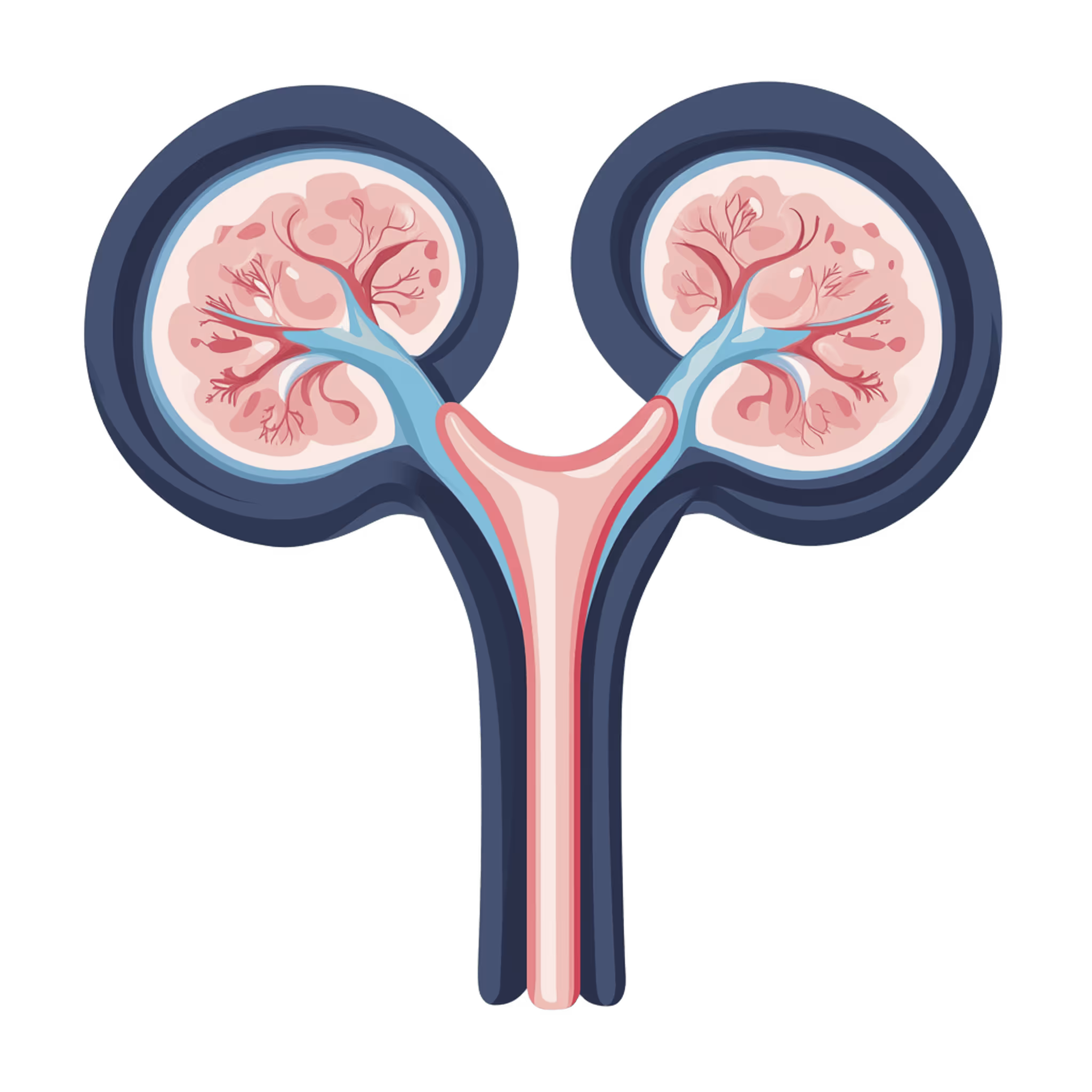
Colorectal (bowel) cancer occurs when abnormal cells in the colon or rectum begin to grow and divide in an uncontrolled way, forming a tumour. The colon and rectum are part of the digestive system, helping to absorb nutrients and remove waste from the body. Most colorectal cancers start as small growths called polyps on the inner lining of the bowel. While most polyps are harmless, some can turn into cancer over time. Colorectal cancer affects both men and women, typically developing after the age of 50.
The symptoms of colorectal cancer can include:
- Persistent changes in bowel habits (such as diarrhoea or constipation)
- Blood in the stool or rectal bleeding
- Abdominal pain, cramping, or bloating
- Unexplained weight loss
- Changes in bowel habits (such as constipation)
- Unexplained weight loss
- Fatigue or weakness
- Feeling that your bowel does not empty completely
These symptoms are common to many less serious conditions, but if they are new, persistent, or frequent, it’s important to see a doctor. Early diagnosis can make a big difference to treatment outcomes. If you are experiencing any symptoms that are worrying you, it is important that you report this to your GP.
Should I Consider Genetic Colorectal Cancer Testing?
If you have a family history of colorectal cancer, or related cancers such as bowel, uterine, or ovarian cancer, you may want to consider colorectal cancer genetic testing. Inherited changes (mutations) in genes such as MLH1, MSH2, MSH6, PMS2, and APC can significantly raise the risk of developing colorectal cancer. Testing can help you find out whether you carry one of these genetic changes, providing valuable information for your future health and your family's.
You might be at higher risk if you have two or more close relatives who have had colorectal cancer, if someone in your family was diagnosed at a young age (under 50), or if you have a known inherited condition like Lynch syndrome or familial adenomatous polyposis (FAP). People of Ashkenazi Jewish descent may also have a higher risk for certain gene mutations linked to colorectal cancer. Research suggests that about 5-10% of all colorectal cancers are caused by inherited genetic changes. Understanding your genetic risk can open up options for early screening, preventative care, or even risk-reducing treatments.
What are the Symptoms?
- Persistent changes in bowel habits (such as diarrhoea or constipation)
- Blood in the stool or rectal bleeding
- Abdominal pain, cramping, or bloating
- Unexplained weight loss
- Changes in bowel habits (such as constipation)
- Unexplained weight loss
- Fatigue or weakness
- Feeling that your bowel does not empty completely
These symptoms are common to many less serious conditions, but if they are new, persistent, or worsening, it’s important to speak to a doctor. Early diagnosis, especially when combined with colorectal cancer genetic screening, can make a big difference to treatment outcomes.
What are the causes?
Usually, when someone is diagnosed with cancer, the cause is unknown. Contributing factors may include age, family history, environment, lifestyle and hormonal factors.
In some cases, genetic testing can identify a variant (change) in a single gene that causes a person to have an increased risk of developing certain cancers over their lifetime. These gene variants can be passed down through families.
One of the most common causes of inherited colorectal cancer is a condition known as Lynch syndrome, which causes an increased lifetime risk of colorectal cancer, endometrial cancer, ovarian cancer and certain other cancers.
Inherited polyposis syndromes, such as Familial Adenomatous Polyposis, which cause someone to develop many polyps in their bowel also increase the chance of developing bowel cancer.
Is genetic testing for colorectal cancer risk genes right for me?
Some people with a personal diagnosis or strong family history of colorectal cancer, bowel polyps or related cancers, such as endometrial or ovarian cancer, may choose to consider genetic testing to try and identify a cause for their diagnosis or their family history.
Identifying a variant in a cancer gene can help clarify personal risk of developing certain cancers and inform your risk management options such as extra screening or medication.
Genetic testing can provide very useful information, but may not be the right choice for everyone. Speaking to a genetic counsellor can help you explore your personal and family history, understand what testing might mean for you and your family, and help you make a decision that feels right for you.